Depression can present in many forms, from mild episodes to major depressive disorder (MDD), the most severe and disabling form. Within this group, treatment-resistant depression is especially difficult to manage since traditional antidepressants, such as SSRIs, often do not work. This has driven the search for fast and effective alternative treatments, such as the administration of ketamine and other psychedelics.
What happens in the brain with depression?
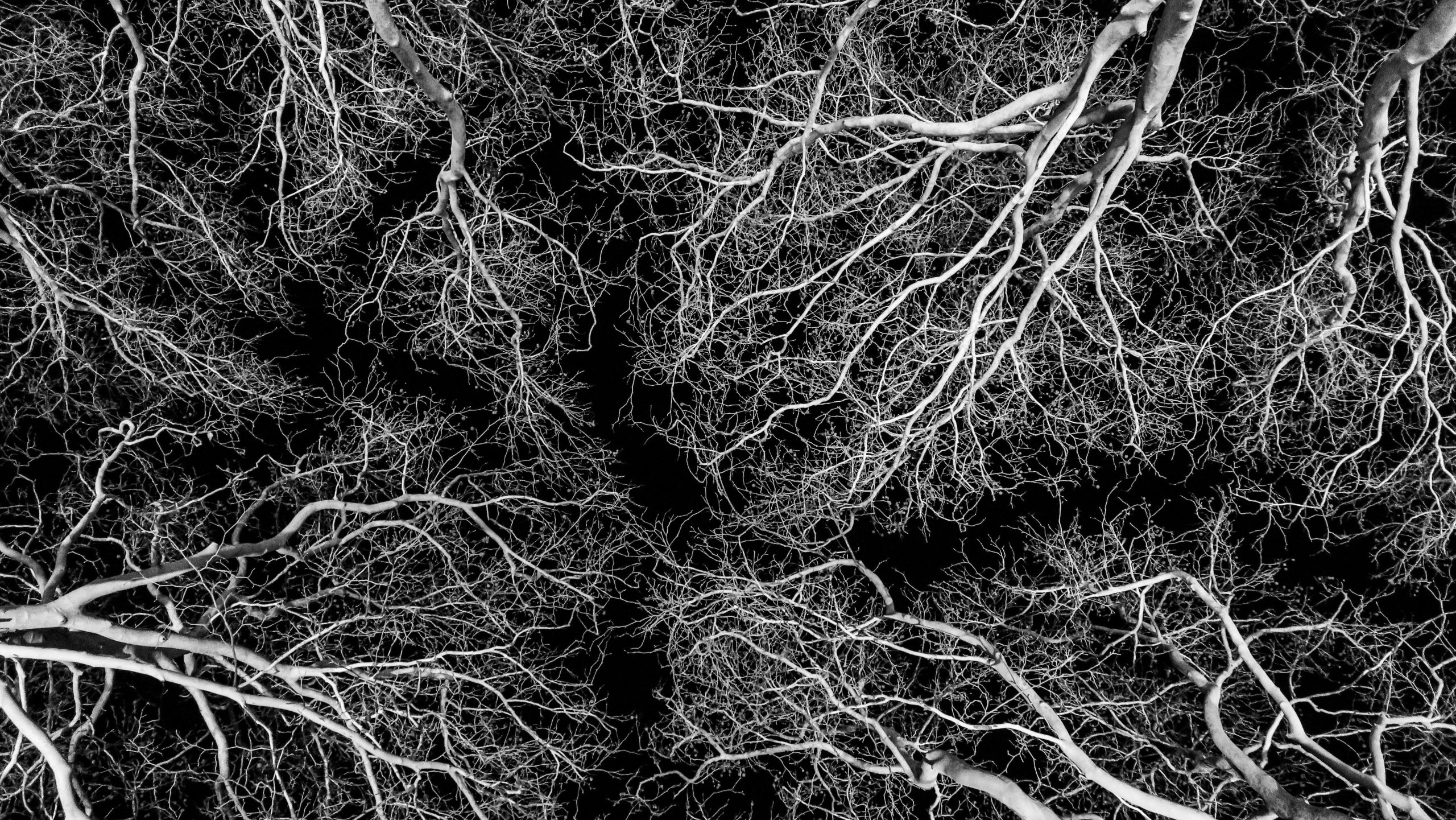
The brain is made up of neurons, which are specialized cells for transmitting information. These neurons communicate through dendritic spines, small protrusions on the neuron whose function is to receive signals from other neurons through synaptic connections.
Anxiety and chronic stress cause the atrophy and retraction of dendritic spines¹², which is considered a risk factor for depression in vulnerable individuals³. In addition, scientific evidence indicates that depression is associated with deficits in information transmission due to the loss of dendritic spines⁴. This neuronal disconnection particularly affects the following areas⁵⁶⁷:
- Hippocampus: plays a key role in memory and learning.
- Subgenual prefrontal cortex: closely related to emotional regulation.
- Anterior cingulate cortex: crucial for attention and decision-making, also involved in emotional regulation.
- Orbitofrontal cortex: implicated in reward evaluation and decision-making.
- Amygdala: closely linked to the processing of emotions such as fear, anxiety, and stress responses.
- Insula: its main function is to integrate bodily sensations and emotions.
Therefore, depression is described as a disorder of cognitive flexibility, generating rumination and rigid negative biases that hinder new forms of learning and adaptive ways of relating to oneself, to others, and to the surrounding environment⁸,⁹.
Neuroplasticity: a flexible brain
For much of the 20th century, it was believed that the adult brain was static and immutable, with fixed synaptic connections after childhood and adolescence. This limited the ability to learn, adapt, or recover from injuries in adulthood.
However, Canadian neuroscientist Donald Hebb (1949) proposed that “neurons that fire together wire together,” suggesting that experience could modify the connections between neurons¹⁰. Later studies in animals and humans demonstrated that learning, environmental stimulation, and rehabilitation could increase the number of synapses and dendritic spines in adult brains¹⁰. Today, this ability of the brain is known as neuroplasticity, defined as the capacity to reorganize and modify its neuronal connections throughout life.
Dendritic spines are a key component of this process, as their size and shape determine the strength and stability of communication between neurons. Some spines are short-lived and disappear within a few days, while others persist for months, consolidating long-lasting neural circuits⁴.
When a new dendritic spine is formed, it can arise in two ways: by activating a previously “silent” area or by being created from scratch. The first allows recovery of previously inaccessible information, while the second establishes new neural networks, increasing flexibility and learning¹¹.
How do ketamine and psychedelics act in the brain?
Animal studies have shown that certain psychedelic substances, including ketamine, can induce synaptic plasticity, with observed changes in the density and size of dendritic spines¹¹.
In the specific case of ketamine, the formation of dendritic spines increases significantly 12 hours after injection and continues up to 72 hours after a single dose¹². Thus, a standard ketamine-assisted therapy protocol—consisting of 2 or 3 administrations of ketamine per week for four weeks—promotes a significant increase in dendrites sustained over a month of treatment. This protocol has shown a significant antidepressant response and complete remission of symptoms in 19.2% of patients with treatment-resistant depression¹³¹⁴.
Regarding anxiety and chronic stress, an increase in spine formation rate has also been observed when ketamine was administered to mice subjected to repeated restraint stress. However, if ketamine is applied prophylactically before the stressor, the ketamine-treated mice are protected against stress-induced spine elimination, acting as a sort of vaccine¹.
In addition to reactivating “silent” dendritic spines, ketamine can stimulate the formation of entirely new spines, allowing neurons to establish connections with new cells¹¹. This implies an increase in brain flexibility and an improvement in the brain’s ability to reorganize its circuits, facilitating the learning of new ways of relating to oneself, to others, and to the environment—ways not previously experienced.
This period of neuroplasticity induced by ketamine and other psychedelics has been linked to critical learning periods¹⁴, which are temporary windows when it is easier to acquire skills or adapt to complex situations. These critical learning periods are easy to understand when we observe how effortlessly a child can learn a new language compared to an adult.
Therefore, it is essential that individuals receiving ketamine-assisted therapy for depression incorporate dynamics, strategies, and healthy habits that support positive change in their daily lives during the treatment process. In this way, during this period of neuronal plasticity, the necessary neural connections will be established to consolidate the desired long-term changes.
References
1. Ng, L. H. L., Huang, Y., Han, M., Iyaswamy, A., Wang, X., Liu, J., … & Song, J. (2018). Ketamine and selective activation of parvalbumin interneurons inhibit stress-induced dendritic spine elimination. Translational Psychiatry, 8(1), 272.
2. Holtmaat, A. J., Trachtenberg, J. T., Wilbrecht, L., Shepherd, G. M., Zhang, X., Knott, G. W., & Svoboda, K. (2005). Transient and persistent dendritic spines in the neocortex in vivo. Neuron, 45(2), 279–291. https://doi.org/10.1016/j.neuron.2005.01.003
3. Lupien, S. J., McEwen, B. S., Gunnar, M. R., & Heim, C. (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience, 10(6), 434–445. https://doi.org/10.1038/nrn2639
4. Thompson, S. M., Kallarackal, A. J., Kvarta, M. D., Van Dyke, A. M., LeGates, T. A., & Cai, X. (2015). An excitatory synapse hypothesis of depression. Trends in Neurosciences, 38(5), 279–294. https://doi.org/10.1016/j.tins.2015.03.003
5. Sheline, Y. I., Wang, P. W., Gado, M. H., Csernansky, J. G., & Vannier, M. W. (1996). Hippocampal atrophy in recurrent major depression. Proceedings of the National Academy of Sciences, 93(9), 3908–3913. https://doi.org/10.1073/pnas.93.9.3908
6. Drevets, W. C., Price, J. L., Simpson, J. R., Todd, R. D., Reich, T., Vannier, M., & Raichle, M. E. (1997). Subgenual prefrontal cortex abnormalities in mood disorders. Nature, 386(6627), 824–827. https://doi.org/10.1038/386824a0
7. Goodkind, M., Eickhoff, S. B., Oathes, D. J., Jiang, Y., Chang, A., Jones-Hagata, L. B., … & Etkin, A. (2015). Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry, 72(4), 305–315. https://doi.org/10.1001/jamapsychiatry.2014.2206
8. Joormann, J. (2010). Cognitive inhibition and emotion regulation in depression. Current Directions in Psychological Science, 19(3), 161–166. https://doi.org/10.1177/0963721410370293
9. Beck, A. T., & Bredemeier, K. (2016). A unified model of depression: Integrating clinical, cognitive, biological, and evolutionary perspectives. Clinical Psychological Science, 4(4), 596–619. https://doi.org/10.1177/2167702616628523
10. Cooper, S. J. (2005). Donald O. Hebb’s synapse and learning rule: A history and commentary. Neuroscience & Biobehavioral Reviews, 28(8), 851–874. https://doi.org/10.1016/j.neubiorev.2004.09.009
11. Liao, C., Dua, A. N., Wojtasiewicz, C., Liston, C., & Kwan, A. C. (2025). Structural neural plasticity evoked by rapid-acting antidepressant interventions. Nature Reviews Neuroscience, 26(2), 101–114.
12. Lüscher, C., & Malenka, R. C. (2011). Drug-evoked synaptic plasticity in addiction: From molecular changes to circuit remodeling. Neuron, 69(4), 650–663. https://doi.org/10.1016/j.neuron.2011.01.017
13. Moda-Sava, R. N., Murdock, M. H., Parekh, P. K., Fetcho, R. N., Huang, B. S., Huynh, T. N., … & Liston, C. (2019). Sustained rescue of prefrontal circuit dysfunction by antidepressant-induced spine formation. Science, 364(6436), eaat8078. https://doi.org/10.1126/science.aat8078
14. Loo, C., Glozier, N., Barton, D., Baune, B. T., Mills, N. T., Fitzgerald, P., Glue, P., Sarma, S., Galvez-Ortiz, V., Hadzi-Pavlovic, D., Alonzo, A., Dong, V., Martin, D., Nikolin, S., Mitchell, P. B., Berk, M., Carter, G., Hackett, M., Leyden, J., … Rodgers, A. (2023). Efficacy and safety of a 4-week course of repeated subcutaneous ketamine injections for treatment-resistant depression (KADS study): Randomised double-blind active-controlled trial. The British Journal of Psychiatry, 223(6), 533–541. https://doi.org/10.1192/bjp.2023.79
15. Singh, J. B., Fedgchin, M., Daly, E. J., De Boer, P., Cooper, K., Lim, P., … & Van Nueten, L. (2016). A double-blind, randomized, placebo-controlled, dose-frequency study of intravenous ketamine in patients with treatment-resistant depression. American Journal of Psychiatry, 173(8), 816–826. https://doi.org/10.1176/appi.ajp.2016.16010037
14. Nardou, R., Sawyer, E., Song, Y. J., Wilkinson, M., Padovan-Hernandez, Y., De Deus, J. L., … & Dölen, G. (2023). Psychedelics reopen the social reward learning critical period. Nature, 618(7966), 790–798. https://doi.org/10.1038/s41586-023-06171-3